The Neuroscience of Trauma
Trauma alters brain structure and function‚ particularly in the amygdala and hippocampus. The amygdala‚ the brain’s fear center‚ becomes hyperactive‚ while the hippocampus‚ responsible for memory processing‚ may malfunction‚ leading to fragmented memories and heightened arousal responses.
1.1 The Brain’s Response to Traumatic Events
The brain’s response to traumatic events involves a rapid activation of the amygdala‚ triggering the fight‚ flight‚ or freeze reaction. Stress hormones like cortisol and adrenaline flood the system‚ preparing the body for immediate action. The hippocampus‚ responsible for memory processing‚ often struggles to consolidate traumatic memories‚ leaving them fragmented and emotionally charged. This disrupts the prefrontal cortex’s ability to regulate emotions and decision-making. The nervous system shifts into hyperarousal‚ making it difficult to return to a state of calm. This biological response is meant to protect but can lead to long-term psychological and neurological challenges if not addressed.
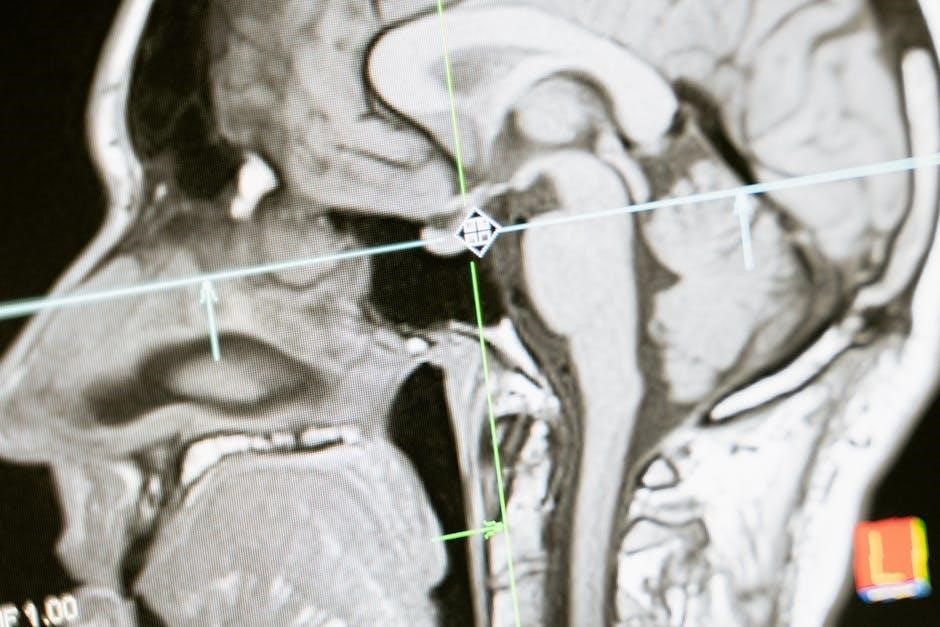
1.2 Changes in Brain Structure and Function
Traumatic experiences can lead to significant changes in brain structure and function‚ particularly in regions like the hippocampus‚ amygdala‚ and prefrontal cortex. The hippocampus‚ crucial for memory formation‚ may shrink due to chronic stress‚ impairing memory processing. The amygdala becomes hyperactive‚ intensifying fear responses. Reduced volume in the prefrontal cortex and anterior cingulate cortex can disrupt decision-making and emotional regulation. These changes disrupt neural communication‚ leading to symptoms like hypervigilance‚ flashbacks‚ and emotional dysregulation. Understanding these alterations is key to addressing the long-term neurological impact of trauma and developing effective interventions.
1.3 The Role of Neuroplasticity in Recovery
Neuroplasticity‚ the brain’s ability to rewire and adapt‚ plays a pivotal role in trauma recovery. By fostering new neural pathways‚ neuroplasticity can help override traumatic memories and restore functional balance. Therapies like cognitive-behavioral therapy (CBT) and mindfulness practices leverage neuroplasticity to enhance emotional regulation and reduce hyperarousal. Over time‚ consistent practice can strengthen healthier neural networks‚ diminishing the intensity of traumatic responses. This adaptive potential underscores the brain’s remarkable capacity for healing‚ offering hope for long-term recovery and resilience.

Psychological and Emotional Impact
Trauma disrupts emotional regulation‚ causing intense fear‚ anxiety‚ and hypervigilance. It can lead to self-preservation behaviors‚ emotional numbing‚ and distorted self-perception‚ profoundly affecting mental health and daily functioning.
2.1 Emotional Regulation and Trauma
Trauma significantly disrupts emotional regulation‚ leading to heightened states of fear‚ anxiety‚ or emotional numbing. The brain’s fear center‚ the amygdala‚ becomes hyperactive‚ while the prefrontal cortex‚ responsible for rational thinking‚ is impaired. This imbalance results in intense emotional reactivity‚ difficulty calming down‚ and challenges in managing stress. Over time‚ survivors may develop hypervigilance or avoidance behaviors to cope with overwhelming emotions. These changes can interfere with daily functioning‚ relationships‚ and overall well-being‚ making emotional regulation a critical area of focus in trauma recovery and healing processes.
2.2 Behavioral Changes and Trauma Responses
Trauma often leads to significant behavioral changes‚ as individuals adopt survival strategies to cope with distress. These may include hypervigilance‚ avoidance of triggers‚ or self-destructive behaviors like substance abuse. In some cases‚ people exhibit impulsivity or aggression‚ while others withdraw socially. These behaviors‚ rooted in the brain’s “fight‚ flight‚ or freeze” response‚ can strain relationships and hinder daily functioning. Trauma survivors may also develop self-preservation habits that‚ while initially adaptive‚ become maladaptive over time. Understanding these responses is crucial for providing compassionate and effective support‚ as they are often misunderstood by others. Tailored interventions can help individuals regain control over their behaviors and emotions‚ fostering a pathway to healing and recovery.

Types of Trauma
Trauma can be acute‚ chronic‚ or developmental‚ each impacting the brain differently. Acute trauma results from single events‚ while chronic trauma stems from prolonged exposure. Developmental trauma occurs during critical growth periods‚ affecting emotional and psychological development. Complex trauma involves multiple‚ interconnected traumatic experiences‚ leading to deep-seated emotional and behavioral challenges. Understanding these distinctions is essential for tailored interventions and support.
3.1 Acute vs. Chronic Trauma

Acute trauma arises from a single‚ discrete event‚ such as a car accident or natural disaster‚ triggering an immediate fight-or-flight response. Chronic trauma‚ however‚ results from prolonged exposure to distressing situations‚ like ongoing abuse or conflict. While acute trauma may resolve with time‚ chronic trauma leads to long-term brain changes‚ including heightened amygdala activity and impaired hippocampal function. This distinction is crucial for understanding the varying impacts on mental health and the need for tailored therapeutic approaches. Recognizing the differences helps in addressing the unique challenges each type presents.
3.2 Developmental Trauma in Children
Developmental trauma occurs when children experience chronic stress or abuse during critical growth periods‚ disrupting brain development. The amygdala becomes hyperactive‚ intensifying fear responses‚ while the hippocampus may malfunction‚ impairing memory processing. This can lead to emotional dysregulation‚ behavioral challenges‚ and difficulty forming healthy relationships. Traumatized children often struggle with impulse control and may exhibit hyperarousal or hypervigilance. Early intervention is crucial to mitigate long-term effects‚ as untreated developmental trauma increases the risk of mental health disorders later in life. Understanding these impacts is vital for providing supportive environments that foster healing and resilience in affected children.

3.3 Complex Trauma and Its Effects
Complex trauma arises from prolonged or repeated exposure to traumatic events‚ often involving interpersonal harm. It deeply impacts the brain‚ altering structures like the amygdala and prefrontal cortex‚ leading to heightened fear responses and impaired emotional regulation. Survivors may experience fragmented memories‚ dissociation‚ and intense emotional dysregulation. Complex trauma also disrupts the body’s stress response system‚ causing chronic hyperarousal or shutdown. These effects can result in long-term mental health challenges‚ including PTSD‚ attachment issues‚ and self-regulation difficulties. Understanding the neurobiological basis of complex trauma is essential for developing effective‚ trauma-informed interventions to support recovery and healing.

Diagnosis and Assessment
Clinical assessment tools‚ such as the Trauma Symptom Inventory and PTSD Checklist‚ help identify trauma-related symptoms. Mental health professionals use these tools to evaluate severity and develop treatment plans.
4.1 Clinical Assessment Tools for Trauma
Clinical assessment tools‚ such as the PTSD Checklist (PCL-5) and the Trauma Symptom Inventory (TSI)‚ are used to evaluate trauma-related symptoms. These tools assess hyperarousal‚ avoidance‚ and dissociation. Mental health professionals administer standardized questionnaires and conduct clinical interviews to identify symptom severity. The process helps differentiate between acute stress and post-traumatic stress disorder (PTSD). Accurate assessment ensures personalized treatment plans‚ addressing specific trauma impacts. These tools are essential for understanding the extent of trauma’s effects on an individual’s mental health and guiding appropriate interventions.
4.2 The Role of Mental Health Professionals
Mental health professionals play a vital role in trauma recovery by providing evidence-based therapies like cognitive-behavioral therapy (CBT) and eye movement desensitization and reprocessing (EMDR). They create safe environments for patients to process traumatic experiences‚ fostering trust and understanding. Professionals also educate clients about trauma’s impact on the brain and body‚ empowering them with coping strategies. Their expertise in diagnosing and treating trauma-related disorders ensures personalized care‚ addressing the unique needs of each individual. By integrating trauma-informed practices‚ they help clients rebuild neural pathways and work toward long-term healing and resilience.

Treatment and Healing
Treatment involves evidence-based therapies like CBT and EMDR‚ alongside trauma-informed care‚ guided by mental health professionals to promote neural recovery and emotional healing.
5.1 Evidence-Based Therapies for Trauma
Evidence-based therapies like Cognitive Behavioral Therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMD) are widely recognized for treating trauma. CBT helps individuals restructure negative thought patterns and behaviors associated with traumatic experiences. EMDR focuses on reprocessing traumatic memories to reduce their distressing effects. Both approaches aim to enhance neural plasticity‚ allowing the brain to heal and reintegrate fragmented memories. These therapies are often conducted under the guidance of trained mental health professionals‚ ensuring a safe and structured environment for recovery. The goal is to restore emotional balance and improve overall well-being.
5.2 Trauma-Informed Care and Practice
Trauma-informed care emphasizes creating a safe‚ non-judgmental environment for survivors‚ acknowledging the prevalence of trauma and its impact. This approach prioritizes trust‚ collaboration‚ and empowerment‚ ensuring care providers understand trauma’s effects on behavior and decision-making. It shifts from asking “What’s wrong with you?” to “What happened to you?” Trauma-informed practices are guided by principles like safety‚ choice‚ and control‚ reducing the risk of re-traumatization. Professionals are trained to recognize triggers and adapt interventions to meet individual needs. This approach is integral in healthcare‚ education‚ and social services‚ fostering resilience and promoting long-term healing and recovery for trauma survivors.
Recovery and Resilience
Recovery and resilience focus on empowering trauma survivors through safe environments and support‚ fostering personal growth and healing.
6.1 Rebuilding Neural Pathways
Trauma disrupts neural pathways‚ but neuroplasticity allows the brain to rewire and heal. Through therapies like mindfulness and cognitive restructuring‚ new connections are formed‚ strengthening resilience. Consistent practice fosters neural recovery‚ helping individuals regain emotional and cognitive balance. This process‚ while gradual‚ demonstrates the brain’s remarkable ability to adapt and recover from traumatic impacts.
6.2 Fostering Resilience in Trauma Survivors
Fostering resilience in trauma survivors involves creating a supportive environment that promotes emotional and psychological healing. Trauma-informed care and mindfulness practices help individuals regain control over their responses to triggers. Building strong social connections and encouraging self-care routines can enhance resilience. Cognitive restructuring and narrative therapy also aid in reframing traumatic experiences‚ reducing their overwhelming impact. By empowering survivors with coping strategies and a sense of purpose‚ resilience is strengthened‚ enabling them to navigate life’s challenges with greater confidence and emotional stability.
Societal and Systemic Implications
Trauma’s societal impact is profound‚ affecting communities and systems. Systemic failures can re-traumatize individuals‚ emphasizing the need for trauma-informed policies to create safer‚ supportive environments.
7.1 Trauma-Informed Systems and Policies
Trauma-informed systems integrate principles that acknowledge the prevalence and impact of trauma. These systems prioritize safety‚ trust‚ and empowerment‚ ensuring that policies minimize re-traumatization. By training professionals and adapting procedures‚ organizations can create environments that support healing rather than exacerbate trauma. Such approaches are essential in healthcare‚ education‚ and justice systems‚ where individuals may be particularly vulnerable. Implementing trauma-informed care at a systemic level fosters resilience and promotes long-term recovery for individuals and communities.
7.2 The Role of Education and Awareness
Education and awareness are critical in addressing trauma effectively. By understanding how trauma impacts the brain and behavior‚ individuals and communities can reduce stigma and promote empathy. Schools‚ workplaces‚ and public programs play a vital role in disseminating accurate information. Training professionals‚ such as teachers and healthcare providers‚ ensures they can identify trauma signs and respond appropriately. Public campaigns and resources‚ like workshops and online materials‚ empower individuals to seek help and support others. Awareness fosters a compassionate society that prioritizes healing and resilience.
Resources and Support
Workbooks‚ guides‚ and online materials provide tools for healing. Organizations like SAMHSA offer trauma-informed care resources‚ while community networks and support groups foster connection and recovery.
8.1 Recommended Reading and Literature
Essential literature includes workbooks like “The Trauma-Informed Practice Guide” and “Healing from Trauma” by A. Hendricks‚ offering practical tools for recovery. SAMHSA’s “Trauma-Informed Care in Behavioral Health Services” provides evidence-based strategies‚ while guides like “Developmental Trauma in Children” address specific trauma types. These resources‚ totaling over 464 pages‚ are designed for both survivors and professionals‚ promoting understanding and healing through structured activities and real-world applications.
8.2 Support Networks and Community Resources
Community resources and support networks play a vital role in trauma recovery. Organizations like SAMHSA and Blue Knot Foundation offer comprehensive programs‚ including the National Center for Trauma-Informed Care and practice guidelines. These resources provide workshops‚ online materials‚ and helplines to aid survivors and professionals.
Initiatives such as the National Trauma Training Programme by NHS Education for Scotland ensure widespread access to trauma-informed care. These networks foster resilience and healing through education‚ advocacy‚ and accessible support services tailored to individual needs.
